Cosa è l’insulino-resistenza?
L’insulino-resistenza è una condizione metabolica causata da fattori quali una dieta ricca di alimenti elaborati e ricchi di carboidrati, uno stile di vita sedentario, un eccesso di grasso corporeo, la genetica e alcune sindromi ormonali come la sindrome dell’ovaio policistico (PCOS) [1].
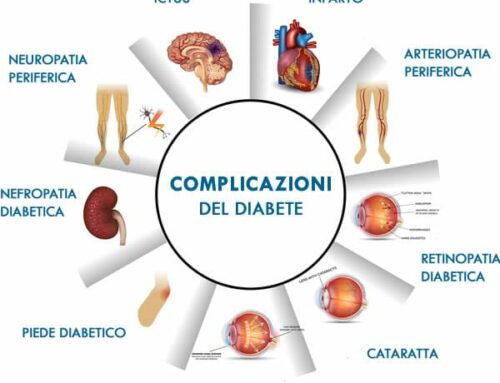
Se non controllata, può progredire verso il pre-diabete, in cui i livelli di zucchero nel sangue sono più alti del normale, e poi verso il diabete di tipo 2, la sindrome metabolica, la malattia del fegato grasso non alcolico e altri problemi cardiovascolari [2-4].
Per comprendere appieno l’insulino-resistenza, è necessario parlare del glucosio, uno zucchero semplice che si trova naturalmente in una varietà di alimenti, tra cui verdure amidacee e cereali come mais, riso, patate e grano, oltre a miele e frutta.
Glucosio e insulina: partner nella gestione dell’energia
Il corpo scompone tutti i carboidrati assunti in glucosio, la sua fonte energetica preferita.
Ci siamo evoluti in modo da dipendere dal glucosio perché è il monosaccaride (zucchero semplice) più abbondante in natura e il più facile da convertire in energia dai mitocondri, i motori delle nostre cellule [6].
In altre parole, il glucosio era essenziale per la nostra sopravvivenza nelle condizioni pre-agricole in cui vivevano i nostri antenati, dove gli alimenti zuccherini e grassi (ipercalorici e ricchi di energia) erano scarsi e i cacciatori-raccoglitori a volte vagavano fino a 500 miglia per cercare cibo [7, 8].
Prima che esistessero i supermercati, i nostri antenati potevano passare gran parte della giornata con poco cibo prima di incontrare una riserva di miele, un gruppo di banane o un altro alimento zuccherino. Per mantenere un apporto costante di energia, il corpo aveva bisogno di immagazzinare calorie aggiuntive per il futuro e si è evoluto per far fronte a questa situazione utilizzando un ormone chiamato insulina [9].
Se pensiamo all’energia come al denaro, l’insulina può essere considerata l’ormone che lo gestisce, alla stregua di un investitore.
 Nella vita, quando si riceve un improvviso afflusso di denaro, si decide, in base a quanto si ha a disposizione e a quanto serve per le spese correnti, se spenderlo, se metterlo in un conto corrente o se metterlo in un conto di risparmio a lungo termine.
Nella vita, quando si riceve un improvviso afflusso di denaro, si decide, in base a quanto si ha a disposizione e a quanto serve per le spese correnti, se spenderlo, se metterlo in un conto corrente o se metterlo in un conto di risparmio a lungo termine.
Nell’organismo, l’insulina svolge un ruolo molto simile, dirigendo il glucosio dove deve andare in base alle esigenze attuali del corpo.
Supponiamo di aver appena mangiato una banana matura e un panino. Ecco cosa succede:
- I livelli di glucosio nel sangue aumentano a causa dell’improvvisa assunzione di carboidrati.
- In risposta a questa “iniezione di liquidità” biochimica, il pancreas (un organo vicino allo stomaco, al fegato e alla cistifellea) rilascia insulina, che trasporta il glucosio nelle cellule attraverso trasportatori specializzati [10, 11].
- Il primo compito dell’insulina è quello di trasportare il glucosio nelle cellule che devono utilizzarlo subito, come le cellule muscolari attive.
- Ma se c’è più glucosio di quello di cui le cellule hanno bisogno per le “spese” correnti (cioè, se c’è più glucosio di quello che è necessario utilizzare immediatamente nelle cellule), l’insulina invia il glucosio per essere accumulato in una molecola di stoccaggio a breve termine chiamata glicogeno. Il glicogeno è come un conto corrente. Immagazzina energia, ma è facilmente scomponibile per prelevarla quando serve. Una piccola quantità di glicogeno è immagazzinata nei muscoli e in altre cellule per il loro uso, ma la maggior parte è immagazzinata nel fegato, dove può essere scomposta in glucosio che viene rilasciato nel sangue per essere utilizzato da tutte le cellule del corpo, comprese quelle cerebrali.
- Una volta riempite le scorte di glicogeno, il glucosio in eccesso che rimane nel flusso sanguigno viene convertito in grasso e immagazzinato nel tessuto adiposo (grasso), che può essere considerato come un conto di risparmio o un fondo per i giorni di pioggia [12]. Sebbene ciò sia naturale, accumulare troppo grasso – in particolare il grasso viscerale, negli organi e attorno ad essi – aumenta il rischio di sviluppare la sindrome metabolica, il diabete, le malattie cardiache e altro ancora.
Perché la resistenza insulinica è importante?
Se l’insulino-resistenza non viene tenuta sotto controllo, può portare a malattie gravi come il diabete di tipo 2, l’aterosclerosi e l’epatosteatosi (fegato grasso) non alcolica [17-19]. Può anche portare a un aumento di peso, che è associato a una serie di esiti negativi per la salute [20].
Gli effetti immediati dell’insulino-resistenza possono avere ripercussioni anche sulle prestazioni quotidiane. Sintomi come sonno insufficiente, stanchezza e difficoltà di concentrazione sono comuni con l’insulino-resistenza e possono rendere difficile il proprio performance-status [21, 22].
Uno dei problemi principali dell’insulino-resistenza è che può innescare un circolo vizioso in cui si sviluppa la voglia di cibi ricchi di carboidrati che compromettono la salute metabolica e peggiorano ulteriormente l’insulino-resistenza [23]. Consumando sempre più alimenti ricchi di carboidrati, i livelli di glucosio si impennano, innescando il rilascio di insulina supplementare da parte del pancreas per riportare i livelli di glicemia alla normalità. Ma poiché le cellule non rispondono all’insulina, si rischia di rimanere bloccati in uno stato di glucosio e insulina elevati, con conseguente aumento di peso e accumulo di grasso difficile da gestire.
Quali sono le cause dell’insulino-resistenza?
Quando consumiamo costantemente una dieta ad alto contenuto di glucosio (un’impresa facile nel mondo moderno, dove abbiamo accesso 24 ore su 24, 7 giorni su 7 a snack e bevande elaborate), il nostro sistema di immagazzinamento basato sull’insulina si stressa.
In sostanza, la capacità di immagazzinare glicogeno nei muscoli e nel fegato si esaurisce e il glucosio in eccesso viene convertito in grasso. Mentre una parte di questo grasso può essere depositata sotto la pelle (grasso sottocutaneo), il corpo deposita anche grasso intorno e dentro agli organi che non è visibile (grasso viscerale). I ricercatori hanno scoperto che uno dei fattori che contribuiscono all’insulino-resistenza è questo tipo di grasso nascosto, che è biologicamente attivo e può rilasciare ormoni e composti infiammatori che promuovono l’insulino-resistenza [13].
La posizione del grasso (sottocutaneo o viscerale) dipende da una serie di fattori, tra cui i geni, il peso alla nascita, gli ormoni e l’età, ma il grasso viscerale è più sensibile ai cambiamenti della dieta e dell’esercizio fisico [37]. In altre parole, il consumo di alimenti elaborati e ricchi di zuccheri e uno stile di vita sedentario possono aumentare il peso e il grasso viscerale, mentre una dieta metabolicamente sana e l’esercizio fisico regolare possono aiutare a metabolizzare il grasso viscerale.
Poiché il grasso viscerale si trova sotto i muscoli della pancia e ricopre gli organi (quindi non si può pizzicare come si farebbe con il grasso sottocutaneo), le persone che non sembrano in sovrappeso possono comunque avere quantità malsane di grasso viscerale e manifestare insulino-resistenza.
A causa degli ormoni e dei composti infiammatori rilasciati dal grasso viscerale, le cellule possono diventare sempre meno reattive all’insulina in termini di assorbimento del glucosio, richiedendo al pancreas di rilasciare sempre più insulina per svolgere lo stesso lavoro. Quando l’insulina perde la sua capacità di trasportare efficacemente il glucosio alle cellule e di mantenere i livelli di glucosio nel sangue entro valori normali, si sviluppa l’insulino-resistenza [13].
È importante sottolineare che non tutti i casi di insulino-resistenza sono legati al consumo eccessivo di zuccheri e che la dieta da sola non è l’unico fattore alla base di una risposta insulinica errata. I ricercatori hanno scoperto che lo stress cronico, un microbioma intestonale disturbato e un sonno non ristoratore sono tutti associati a un rischio maggiore di sviluppare l’insulino-resistenza.
Il rischio di insulino-resistenza aumenta con l’età?
L’invecchiamento comporta una serie di cambiamenti fisiologici, alcuni dei quali sono visibili (come le rughe e i capelli brizzolati) e altri no. In effetti, con l’avanzare dell’età aumenta il rischio di sviluppare insulino-resistenza (o ridotta sensibilità all’insulina), indipendentemente dal fatto che si conduca o meno uno stile di vita metabolicamente sano. In altre parole, si possono fare tutte le cose “giuste” dal punto di vista metabolico, ma la sensibilità all’insulina può essere ridotta.
Anche altri aspetti dell’invecchiamento sono associati all’insulino-resistenza. La diminuzione dei livelli di estrogeni durante la menopausa, ad esempio, può rendere le cellule meno reattive all’insulina e portare a livelli più elevati di glucosio nel sangue. Inoltre, sia la menopausa che l’andropausa (un calo degli ormoni sessuali negli uomini legato all’età) possono portare a una riduzione della massa muscolare, a un aumento del grasso viscerale e ad altri cambiamenti nella composizione corporea che possono influire sulla sensibilità all’insulina.
Nuove ricerche suggeriscono anche forti legami tra la resistenza insulinica nel cervello e lo sviluppo del morbo di Alzheimer, che a volte viene chiamato “diabete di tipo 3”.
Qual è il rapporto tra insulino-resistenza e PCOS?
L’insulino-resistenza è associata alla sindrome dell’ovaio policistico, o PCOS. La PCOS è un disturbo ormonale caratterizzato dalla presenza di cisti ovariche che possono interrompere le mestruazioni e la fertilità, anche se spesso si accompagna a complicazioni come l’insulino-resistenza, l’aumento del rischio di problemi cardiovascolari, l’aumento di androgeni (ormoni sessuali maschili) e di grasso addominale. Gli scienziati ha e che tale resistenza può di fatto contribuire allo sviluppo della PCOS [33].
Quali sono i segni e i sintomi dell’insulino-resistenza?
Alcune persone affette da insulino-resistenza presentano segni evidenti, come [14, 15]:
- uno scurimento della pelle intorno alle ascelle o al collo, noto come acantosi nigricans
- piccole escrescenze cutanee (legate alla pelle) chiamate “skin tag” o altre anomalie cutanee
- un girovita allargato (“forma a mela”).
Se la situazione è diventata più grave e si è passati all’iperglicemia (glicemia alta), ci si può sentire stanchi e assetati, con necessità di urinare frequentemente, o affamati anche se si ha già mangiato [16].
L’insulino-resistenza può avere segnali di allarme insoliti o sorprendenti che non sono così evidenti, tra cui:
- Perdita di capelli, dovuta agli elevati livelli di glucosio nel sangue che modificano il ciclo di crescita dei capelli e innescano un’infiammazione che impedisce il flusso sanguigno ai follicoli piliferi.
- Voglia di zucchero, dovuta a un circolo vizioso in cui il glucosio del corpo è disregolato e si inizia a desiderare cose dolci per riportare i livelli di glucosio alla normalità dopo il crollo.
- Letargia e affaticamento, dovuti al fatto che le cellule sono affamate di glucosio e non sono in grado di utilizzarlo correttamente.
La realtà è che la maggior parte delle persone affette da insulino-resistenza non presenta sintomi evidenti, il che rende ancora più importante consultare il medico per gli esami del sangue di routine e condurre uno stile di vita equilibrato e metabolicamente sano.
Come si diagnostica l’insulino-resistenza?
Il modo migliore per capire se si è sviluppata una resistenza insulinica è fare un esame del sangue.
I tre test più comuni sono:
- Il test del glucosio e dell’insulina a digiuno, che misura i livelli di glucosio dopo almeno 12 ore senza mangiare o bere. L’HOMA-index ci fornisce l’insulino-resistenza attraverso il calcolo: glicemia x insulina/405.
- Il test di tolleranza orale al glucosio, in cui si esegue il test del glucosio plasmatico a digiuno, si beve una soluzione speciale di glucosio e si misurano i livelli di glucosio nel sangue ogni 30 minuti per 2 ore. In questi casi preferisco sempre calcolare oltre alla glicemia anche il valore dell’insulina ad ogni prelievo.
- Un test dell’emoglobina A1C, che fornisce un quadro dell’andamento glicemico degli ultimi 3 mesi.
Quali sono i trattamenti disponibili per l’insulino-resistenza?
Il modo migliore per trattare l’insulino-resistenza è apportare modifiche allo stile di vita in relazione alla dieta, all’esercizio fisico, al sonno e allo stress (vedi sotto). Ma il medico può decidere di prescrivervi la metformina, un farmaco che sensibilizza le cellule all’insulina e aiuta a mantenere equilibrati i livelli di glucosio nel sangue [36]. La metformina, come l’Ozempic e altri agonisti del GLP-1, è comunemente utilizzata per il trattamento del diabete di tipo 2. Non viene utilizzata esplicitamente per trattare l’insulino-resistenza, ma può contribuire a migliorarne i sintomi.
Come si inverte la resistenza all’insulina?
accorgimenti alla portata di tutti per invertirla. I due elementi chiave per invertire l’insulino-resistenza sono (1) migliorare la sensibilità all’insulina e (2) stabilizzare i livelli di glucosio nel sangue, prestando molta attenzione ai quattro pilastri:
- dieta,
- esercizio fisico,
- sonno e
- stress.
1. Mangiare una dieta metabolicamente sana
L’alimentazione ha un potente effetto sull’insulino-resistenza. Ciò che si mangia – e soprattuto quando – può aiutare a stabilizzare i livelli di zucchero nel sangue e ad evitare le montagne russe del glucosio (i famosi picchi glicemici con conseguente caduta della glicemia e sensazione di attacco di fame di dolce), che possono rapidamente degenerare in una ridotta sensibilità all’insulina.
Quando si tratta di costruire un piatto metabolicamente sano, il consumo di fibre è importante. Le fibre sono un ottimo modo per abbassare i livelli di glucosio nel sangue e ridurre il rischio di sviluppare insulino-resistenza [30].
Altri aspetti fondamentali di una dieta che può aiutare a invertire la resistenza all’insulina:
- Mangiare proteine e grassi sani per ottenere il senso di sazietà.
- Evitare gli alimenti processati e lo zucchero raffinato
- Sperimentare l’orario dei pasti e il digiuno intermittente (consiglio di saltare la cena)
- Evitare la colazione ricca di carboidrati: ne consegue un andamento glicemico durante il giorno meno controllato e più fame. Su Marte tutti i sostituti del latte e sostituti di pasto. la miglior colazione è una colazione proteica e grassa.
2. Esercizio fisico regolare
Se l’alimentazione può aiutare a bilanciare i livelli di glucosio, l’esercizio fisico è il modo migliore per migliorare la sensibilità all’insulina. Secondo uno studio, anche una sola sessione di esercizio fisico moderato può migliorare la sensibilità all’insulina fino a 48 ore [35]. Un altro studio del 2017 ha rilevato che anche meno di un’ora di allenamento di resistenza a settimana (senza esercizio aerobico aggiuntivo) riduce il rischio di sviluppare la sindrome metabolica [26]. Un altro gruppo di studi ha rilevato che 2-3 sessioni di allenamento di resistenza per almeno 8 settimane hanno migliorato la sensibilità all’insulina fino al 48% [27].
Quando si fa esercizio fisico, il corpo “rompe” il glicogeno e libera il glucosio da bruciare durante l’esercizio, che a sua volta libera spazio di “stoccaggio”. Questo spazio può essere utilizzato per immagazzinare ancora più glucosio durante il prossimo pasto ricco di carboidrati, invece di costringere l’insulina a dirigerlo verso le cellule adipose.
Sebbene ogni tipo di esercizio sia utile per la salute del metabolismo, praticare un mix di allenamento di resistenza e di esercizio aerobico può aiutare a migliorare la composizione corporea e a costruire muscoli (che utilizzano più glucosio in circolo: ricordate che l’80% del glucosio circolante finisce nei muscoli, finchè c’è spazio per il glicogeno).
Cinque dei migliori esercizi per l’insulino-resistenza sono:
- Camminare veloci
- Corsa
- Nuoto
- Pesi
- Corsa
Per quanto riguarda l’orario dell’allenamento, il momento migliore è quello in cui ci si allena con costanza. Tuttavia, alcune ricerche preliminari suggeriscono che gli allenamenti mattutini sono più adatti alla perdita di peso e alla concentrazione/attenzione, mentre gli allenamenti serali possono avere un effetto maggiore sulla salute metabolica.
3. Dormire un sonno di qualità
Il sonno è fondamentale per la sensibilità all’insulina, l’equilibrio dei livelli di glucosio e la salute metabolica in generale. Una sola notte di cattivo sonno può provocare un aumento misurabile dell’insulino-resistenza in persone sane [28]. Ma per dormire bene sono necessari alcuni fattori, tra cui la tempistica e la variabilità del sonno. In altre parole, non solo l’ora in cui si va a letto e ci si sveglia, ma anche la costanza della routine del sonno.
Una systematic review del 2020 ha rilevato che tempi di sonno più tardivi e una maggiore variabilità del sonno sono associati a un aumento del rischio cardiometabolico e ad altri esiti negativi per la salute [29].
Per migliorare la qualità del sonno, è importante praticare una buona igiene del sonno. Questo include:
- Evitare di mangiare (soprattutto i carboidrati) prima di andare a letto.
- Mantenere la stanza fresca, tra i 15 e i 19°C.
- Spegnere gli schermi almeno un’ora prima di andare a letto
- Prendere la luce diretta del sole entro 2 ore dopo essersi svegliati.
- Utilizzare tende oscuranti o maschere per gli occhi
- Eliminare la caffeina dopo pranzo
4. Gestire lo stress
Lo stress cronico, in cui i livelli del cortisolo sono elevati per un lungo periodo di tempo, può favorire l’insulino-resistenza e compromettere la salute metabolica. Ciò è dovuto in parte al fatto che il cortisolo può naturalmente ostacolare la secrezione di insulina, anche se questo non rappresenta un problema significativo nei casi di stress acuto e di breve durata [32].
Nel tempo, lo stress può contribuire all’insorgenza di insulino-resistenza, danneggiando le cellule beta pancreatiche (responsabili della produzione di insulina) e innescando un’infiammazione diffusa che peggiora l’insulino-resistenza. Può anche spingere a fare scelte sbagliate per la salute del metabolismo, come fare spuntini a base di cibi elaborati e dolci e fare meno esercizio fisico, il che ci blocca in un circolo vizioso metabolico.
Oltre a ridurre lo stress attraverso l’esercizio fisico (anche solo due giorni a settimana di esercizio aerobico possono aiutare a ridurre l’ansia), gli studi dimostrano che le pratiche di mindfulness come la meditazione possono aiutare a ridurre la risposta fisiologica allo stress [34].
5. Mantenere un peso corporeo adeguato
L’insulino-resistenza può portare a un aumento di peso, che può ulteriormente peggiorare l’insulino-resistenza, causando un circolo vizioso difficile da interrompere.
Uno studio condotto su donne adulte di età compresa tra i 24 e i 40 anni ha rilevato che coloro che avevano mantenuto il peso perso dimostravano una maggiore sensibilità all’insulina rispetto al gruppo di controllo senza storia di perdita di peso [24].
D’altro canto, le donne che avevano perso peso in precedenza, ma che poi lo avevano riacquistato, mostravano una ridotta sensibilità all’insulina. I ricercatori che hanno studiato donne in sovrappeso e obese hanno scoperto che il mantenimento di una riduzione del 15% del peso corporeo per 12 mesi ha migliorato la sensibilità all’insulina [25].
Questo non significa che non si possa perdere peso in modo efficace in presenza di insulino-resistenza, ma che quando ci si concentra principalmente sull’inversione dell’insulino-resistenza (cioè sull’equilibrio dei livelli di glucosio e sul miglioramento della sensibilità all’insulina), la perdita di peso diventa un effetto collaterale naturale del percorso.
Come può aiutarvi un CGM a risolvere l’insulino-resistenza?
Se i due passi fondamentali per invertire l’insulino-resistenza sono il miglioramento della sensibilità all’insulina e l’equilibrio dei livelli di glucosio, il monitoraggio continuo del glucosio (CGM) è uno strumento potente per aiutarvi a monitorare i livelli di glicemia in modo costante e in tempo reale. Il monitoraggio dei livelli di glicemia tramite il CGM abbinato a un’applicazione sul vostro cellulare può fornirvi un’ampia gamma di informazioni che consentono di apportare modifiche specifiche e a lungo termine allo stile di vita, molte delle quali possono migliorare la sensibilità all’insulina.
Non solo si può imparare a identificare gli alimenti che scatenano i picchi glicemici, ma si può anche capire come le proprie risposte specifiche ai tempi dell’esercizio fisico, ai modelli di sonno e ai periodi di stress o inattività contribuiscano a influenzare livelli di glicemia e di conseguenza anche della risposta insulinica.
Soprattutto l’impiego del CGM può fornire le conoscenze necessarie per combattere l’insulino-resistenza prima che si trasformi in una condizione cronica più grave come il diabete di tipo 2. Poiché i sintomi del disordine metabolico spesso non compaiono fino a quando non è troppo tardi, molte persone con insulino-resistenza non sanno nemmeno di averla.
In pratica cosa vi consiglio di fare?
L’insulino-resistenza è una delle principali cause alla base delle malattie croniche del nostro secolo.
Qualche consiglio pratico, anche per accelerare il metabolismo:
1. Mangiare proteine e grassi prima dei carboidrati non provoca picchi glicemici. Ricordate che le fibre vi riducono anch’esse i picchi glicemici (verdure). La dieta LOW CARB è l’approccio ideale, specie se associato al digiuno intermittente.
2. Fare una passeggiata dopo i pasti può aiutare ad abbassare la risposta glicemica e a prevenire i picchi glicemici: entro 90 minuti.
3. Gli allenamenti ad alta intensità possono effettivamente causare un aumento della glicemia a causa del rilascio da parte del fegato di una maggiore quantità di glucosio da utilizzare come energia per i muscoli durante l’allenamento, ma questi aumenti non sono dannosi e finiscono per aiutare a stabilizzare la glicemia a lungo termine.
4. La terapia del freddo è una nuova tecnica per il recupero dopo l’allenamento e può aiutare ad abbassare i livelli di glicemia dopo una sessione intensa.
5. Le tecniche di gestione dello stress sono importanti, poiché sappiamo che lo stress cronico e a breve termine provoca un aumento dei livelli di zucchero nel sangue.
6. L’uso di aceto di mele in acqua (1 cucchiaio) prima del pasto riduce il picco glicemico.
7. Poichè il peso influisce sulla risposta all’insulina, raggiungere un peso corporeo adeguato è cruciale.
8. Sonno di qualità.
Per scrivere l’articolo mi sono basata sulla pubblicazione di Claudia S. Copeland, PhD
Bibliografia:
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1204764/
- https://www.niddk.nih.gov/health-information/diabetes/overview/what-is-diabetes/prediabetes-insulin-resistance
- https://www.cdc.gov/diabetes/basics/type2.html
- https://www.ncbi.nlm.nih.gov/books/NBK507839/
- https://academic.oup.com/jcem/article/107/1/e25/6362635
- https://www.sciencedirect.com/topics/nursing-and-health-professions/monosaccharide
- https://www.veri.co/learn/the-science-behind-sugar-cravings
- https://education.nationalgeographic.org/resource/hunter-gatherer-culture
- https://pubchem.ncbi.nlm.nih.gov/compound/Insulin-human
- https://www.ncbi.nlm.nih.gov/books/NBK279306/
- https://pubmed.ncbi.nlm.nih.gov/31175156/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4985254/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8831809/
- https://pubmed.ncbi.nlm.nih.gov/31261473/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8106409/
- https://www.cdc.gov/diabetes/managing/manage-blood-sugar.html
- https://www.cdc.gov/diabetes/basics/type2.html
- https://pubmed.ncbi.nlm.nih.gov/31050706/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5409726/
- https://www.veri.co/post/insulin-resistance-and-weight-loss
- https://sleepwhispererpodcast.com/027-insulin-resistance-sleepwith-dr-benjamin-bikman
- https://pubmed.ncbi.nlm.nih.gov/20102774/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3554293/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5519190/
- https://www.healio.com/news/endocrinology/20170623/maintained-weight-loss-for-1-year-increases-insulin-sensitivity-in-women
- https://www.mayoclinicproceedings.org/article/S0025-6196(17)30167-2/fulltext
- https://bmjopensem.bmj.com/content/2/1/e000143
- https://pubmed.ncbi.nlm.nih.gov/20371664/
- https://cdnsciencepub.com/doi/10.1139/apnm-2020-0032
- https://www.fda.gov/food/food-labeling-nutrition/questions-and-answers-dietary-fiber#beneficial_physiological_effects
- https://academic.oup.com/ajcn/article/94/2/459/4597854?login=false
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4919480/
- https://pubmed.ncbi.nlm.nih.gov/22192137/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5526744/
- https://www.scielo.br/j/rbme/a/HTX3GCF4FFwkD85trLSvFgm/?lang=en&format=pdf
- https://diabetes.org/healthy-living/medication-treatments/insulin-resistance
- https://www.health.harvard.edu/staying-healthy/taking-aim-at-belly-fat